HIV is a virus that is spread through semen, vaginal fluids, blood and breast milk. HIV transmission can happen during sex, when injection equipment is shared, between a mother and baby, or during other activities when bodily fluids are exchanged between a person living with HIV and a person who is HIV-negative. There are a number of ways to prevent HIV infection.
TREATMENT AS PREVENTION
One of the most effective ways to prevent HIV transmission is called “treatment as prevention” or TasP. It’s when a person living with HIV stays on treatment, their viral load can become so low that it’s “undetectable” and they do not transmit the virus to others.
How does TasP work? Today’s HIV medications work to block the replication of the virus. When a person living with HIV takes medications as prescribed, treatment lowers the amount of virus in their body (their viral load decreases). It’s possible for a person living with HIV to have a viral load so low that it cannot be detected by viral load tests. That’s what “undetectable” means. Typically, people who have viral loads less than 50 copies/mL (<50 copies/mL) are considered to be undetectable.
When people living with HIV are undetectable, they do not transmit HIV.
Read more about what it means to be undetectable.PrEP
PrEP stands for pre-exposure prophylaxis. PrEP is a method of HIV prevention where people who are HIV-negative take a medication to prevent HIV infection. PrEP is very effective at preventing HIV infection when used as prescribed. There are different ways to take PrEP, which you can read about here. Truvada, Descovy, and Apretude are all medications taken for PrEP.
Pro tip: People also use the word “PrEP” when describing the actual medication that they take when they’re using pre-exposure prophylaxis as a prevention method. So, sometimes it refers to either the method or the medication.
How does PrEP work? An HIV-negative person takes PrEP as prescribed by their provider. PrEP works by blocking an enzyme that HIV needs in order to make copies of itself. Without the ability to replicate, the virus is unable to take hold and is cleared from the body.
So, if an HIV-negative person who is taking PrEP has condomless sex with a person living with HIV who does not have an undetectable viral load, they will be exposed to the virus, but PrEP works by preventing HIV from replicating in their body.
It’s important to remember that PrEP is highly effective, but PrEP is not 100% effective in preventing HIV. And, PrEP does not prevent STIs.
PEP
PEP stands for post-exposure prophylaxis. PEP is an emergency treatment for people who have been exposed to HIV. If you have been exposed to HIV in the previous 72 hours, talk with a medical provider right away.
The sooner you start taking PEP, the better. PEP is effective in preventing HIV when taken correctly, but not 100 percent.
PEP involves taking a series of pills for 28 days to prevent HIV infection. For PEP to work, you must start PEP within 72 hours of a possible exposure — the sooner PEP is started, the more likely it will be effective.
If you think you have been exposed to HIV, go to an emergency room or healthcare provider right away.
Read more about PEP.CONDOMS & LUBE
Using condoms and water- or silicone-based lube every time you have sex can help prevent HIV. Condoms also help prevent the spread of STIs including syphilis, gonorrhea and chlamydia. You can use external condoms (that go over a penis) and internal condoms (that can go inside a vagina, front hole or butt) to prevent HIV and STIs.
Make sure you use a water- or silicone-based lube with condoms, not oil-based lube. Oil-based lubricants can cause condoms to break.
Get free condoms, lube, dental dams and other safer sex supplies.SAFER DRUG USE
HIV can be transmitted from one person to another during injection drug use if needles or syringes are shared. Sharing syringes with another person is considered a “high risk” activity for HIV and hepatitis C transmission.
Using new, sterile syringes every time you inject and not sharing injection equipment and works (cotton, water, cookers, etc.) with other people prevents HIV and hepatitis C transmission.
Get access to syringes, proper disposal containers and other safer consumption supplies.More HIV Resources
More Sexual Health Resources

Sexual Health Brochures
Check out our collection of gender-inclusive STI brochures--available to download, for free...

PrEP Facts: Introduction & FAQ
Learn more about Pre-Exposure Prophylaxis (PrEP) and how this HIV prevention strategy may be useful for you or someone you know.

Landscape of Options for Oral PrEP
A generic version of a medication used for oral PrEP is now available. Here’s what to know — and what to do if you run into any payment issues at the pharmacy.

Info sheet: Which PrEP medication is best for me?
Two different medications are now FDA-approved for PrEP in the US: Truvada and...

Side-by-side comparison: Truvada and Descovy for PrEP
There are now two medications approved by the US Food and Drug Administration (FDA) for PrEP:...
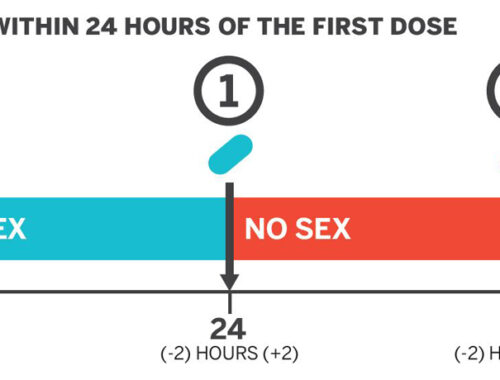
Info sheet: PrEP 2-1-1
Find out more info about how to take Truvada for PrEP 2-1-1 with this downloadable info...

Q&A: PrEP 2-1-1
Get answers to your questions about PrEP 2-1-1 or PrEP “on-demand” with expertise from three clinicians.

HIV Today Infographic
San Francisco has made incredible progress in reducing HIV transmission, but not everyone has benefited equally. Find out what we must do to get to zero.





