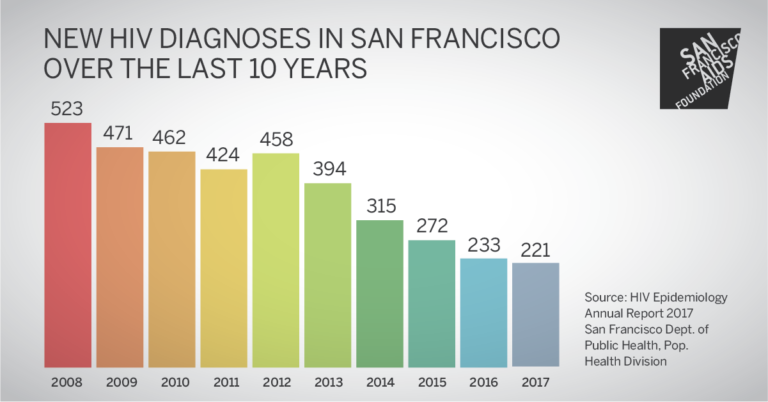
SF reaches new historic low number of HIV infections in 2017

The number of HIV infections happening in San Francisco continues to decline, with a record low number of HIV infections occurring in 2017 than ever before. The rate of decline, however, is slowing. As new data from the 2017 HIV Epidemiology Annual Report reveals, homeless people, people of color, trans women and people who use injection drugs are particularly affected.
“San Francisco has made incredible progress over the last decade reducing the number of new HIV infections. More people know their HIV status than ever before, and a greater share of people living with HIV are virally suppressed,” said Joe Hollendoner, CEO of San Francisco AIDS Foundation. “But we have much more work to do as disparities continue especially among African Americans, Latinx individuals, and people experiencing homelessness. Our vision of achieving the goals of getting to zero is closer than ever but in order to end AIDS we must continue to innovate upon HIV prevention and care services to ensure that no community gets left behind.”
5% decline in new HIV infections
In 2017, a total of 221 people were diagnosed with HIV in San Francisco. This represents a 5% decrease in the number of new HIV infections since the previous year, when 233 people were diagnosed. In previous years the percent reduction in HIV diagnoses was closer to 14% to 16%.
Susan Scheer, PhD, MPH, from the San Francisco Department of Public Health, noted that there were six populations that showed no declines in new HIV infections in recent years: African Americans, Asians, women, people who use injection drugs, men who have sex with men with a history of injection drug use and people who are homeless.
“San Francisco is doing an amazing job, and we have seen such change in recent years, but there are really important populations that we’re not reaching,” said Tracy Packer, MPH, from the San Francisco Department of Public Health.
HIV infection rates—which show HIV infections relative to population size—reveal disparities among communities of color. African American men (116 infections per 100,000) and African American women (43 infections per 100,000) continue to be disproportionately affected by HIV. (The infection rates in 2017 for white men and white women were 39 per 100,000 and 10 per 100,000, comparatively.)
HIV rates among African American women have increased since 2014 (from 5 per 100,000 in 2014 to 43 per 100,000 in 2017). The rate among African American men has increased over the past year, from 98 per 100,000 in 2016 to 116 per 100,000 in 2017.
Since 2006, HIV infections have declined the most among people who are white and also men who have sex with men—mirroring data on PrEP uptake.
The city now estimates that between 16,000 and 20,000 men who have sex with men are using PrEP in San Francisco (up from an estimated 12,600 in 2016; 10,000 in 2015; and 4,400 in 2014). Among San Francisco City Clinic PrEP clients, African Americans had the lowest proportion of PrEP use (34%) compared to clients who were white (50%), Latino (48%) and Asian (49%).
Among PrEP clients at community-based organizations including San Francisco Community Health Center, LYRIC, San Francisco AIDS Foundation, Instituto de la Raza and Alliance Health Project, Latino men who have sex with men were the most likely to start PrEP after being screened (58%). Trans women (25%) and African American men who have sex with men (44%) were the least likely to choose to begin PrEP.
HIV testing, care and viral suppression
San Francisco continues to make gains in the number of people that quickly get diagnosed, linked to HIV care and virally suppressed (which is best for individual health and also HIV prevention).
An estimated 94% of people living with HIV are diagnosed and aware of their status, which Scheer described as “very high” compared to the national average of 86%.
Among people newly diagnosed in 2016, 83% were linked to care within one month of their diagnosis, 71% were retained in care for three to nine months after diagnosis and 85% were virally suppressed within one year.
Among all people living with HIV known to reside in San Francisco, a number of populations had rates of viral suppression lower than the 74% average: women, trans women, African Americans, Latinos, people under age 50, people who use injection drugs, men who have sex with men who use injection drugs, and people who are homeless. The rate of viral suppression among people who are homeless was particularly low, at 32%.
“People experiencing homelessness have the lowest viral suppression rates of any population – less than half the average rate of San Franciscans living with HIV,” said Hollendoner. “Until there is more permanent supportive housing in San Francisco, we will continue to see this disparity. Housing is an effective strategy in ending the HIV epidemic as it has not only proven to improve viral suppression rates, it also prevents new infections from occurring. Bottom line: housing is health care.”
—