Drug Quality Testing
By John Halifax, Health Educator
Currently, we are investigating two different types of chemical laboratory instruments to use for drug quality testing. The first is a machine called a Fourier Transformation Infrared Spectrometer (FTIR), which uses a laser to bombard the sample with different wavelengths of infrared light. For a particular chemical, specific infrared light waves will cause the bonds between atoms to “wiggle.”
In causing a chemical bond to wiggle, the infrared wave is absorbed, and the output of an FTIR scan is a graph showing what infrared light waves were absorbed by the sample. This graph, called a spectrum, can be thought of as the molecule’s “fingerprint.”
If a drug sample is a mix of different substances, an FTIR spectrometer can scan the sample, and software can compare the sample’s “fingerprint” to a database of fingerprints of pure chemicals to determine what is in the sample and the ratio of the sample’s components (i.e. a cake is 20% butter, 45% flour, 20% sugar, 10% eggs, and 5% other stuff). FTIR is a relatively cheap and easy way to test a sample and is non-destructive (the participant will get back any sample they provide for testing).
The other instrument we are looking into is called a Mass Spectrometer. Mass Spectrometry (MS) is a technique where the sample molecule is magnetically charged, typically by bombarding the sample with electrons. This process often causes the molecule to break into fragments. These fragments also have a magnetic charge, and a magnet separates these fragments based on their size. Molecules have typical fragmentation patterns, and these can be used to identify what the sample is.
A key step in MS is that before fragmentation happens, a sample has to be separated into the individual components that make it up. For example, if you were testing a white powder that was half salt, half baking soda, you would need to first separate the salt in the mixture from the baking soda, and then test the salt and baking soda individually in the MS. This required separation step means that any sample for MS requires more preparation than FTIR, and there are different methods that can be used to separate the sample. Mass spectrometry provides more precise information than FTIR, but it is typically more expensive and harder to use. Mass spectrometry is also a destructive method, so a participant will not get back the sample they provide. Currently, we are exploring both types of instruments to see what will best meet our needs, and what can best serve our participants.
Syringe Programs in Prisons
By Andrew Reynolds, HCV Program Manager
Did you know that there are needle exchange programs in jails and prisons throughout the world? There are none in the United States, mind you, but prison-based syringe programs have been found to be safe and effective while reducing injection drug use-related problems both for the people living in and using drugs as well as those who work in these settings. The first needle exchange program in prisons started in 1992. Dr. Franz Probst was working in the Oberschogrum prison for men in Switzerland, and he was faced with a dilemma: He had patients who were injecting drugs inside and he knew they had no access to unused injecting equipment.
Rather than turn in these men to prison authorities, he mounted an act of civil disobedience and started giving out sterile syringes. When he got caught and brought the prison director, he made an impassioned plea for the health and safety of his patients, argued for the benefits of HIV and HCV prevention, reduction in soft tissue infections and other medical complications related to injection drug use, and rather than get fired, he convinced them to make it legal!
Today, there are 60 prisons around the world that have syringe service programs. Now, there are over 10,000 prisons worldwide so there remains a significant need to expand harm reduction services and programs, but we are moving in the right direction. We need them in the United States, too: Data is hard to come by, but reports of overdose deaths, HIV and HCV transmission in prisons are proof enough that drug use happens behind prison walls. Just as harm reduction services like SSPs, naloxone distribution and medication-assisted treatment (MAT) work outside, they can and do work inside. In a perfect world, we wouldn’t arrest and imprison people who use drugs, but if we do, we should provide them with the things they need to stay safe and healthy.
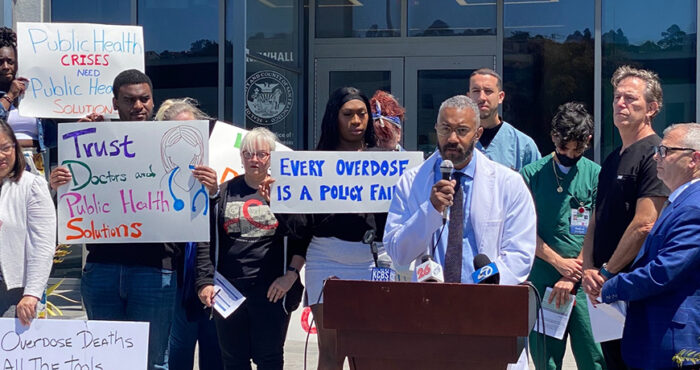
Harm Reduction Policy Update
By Laura Thomas, Director of Harm Reduction Policy
As with everything else this year, it was a strange time in the state legislature, and many bills were put off until next year. San Francisco AIDS Foundation co-sponsored three harm reduction bills in the state legislature. One of them, AB 2077 (Ting) is currently on the Governor’s desk awaiting his signature. It will extend the ability of pharmacists to sell syringes without a prescription and further decriminalize syringe possession for individuals. That’s the good news. The other two bills did not move forward in the COVID shortened session and will have to be reintroduced next year. The biggest disappointment is that AB 362 (Eggman), the bill to allow San Francisco and Oakland to open supervised consumption services, didn’t get voted on and died at the end of the session. It’s particularly frustrating because we had the votes to pass it and because the need is even more urgent right now as overdose deaths go up in San Francisco. We will bring it back next year and Senator Wiener has already said he’s planning to introduce a bill and hopefully pass it so we can start providing these life-saving services in San Francisco. The other bill, SB 888 (Wiener), would have supported contingency management, such as what SFAF provides through PROP.
Around the state, syringe access programs are facing NIMBY pressure and some have had to close. Northern Valley Harm Reduction in Chico was sued by local neighbors and agreed to stop providing syringe access, although they are still doing outreach and distributing naloxone. Santa Ana, Eureka, and Santa Cruz are also facing threats and legislation. However, new programs are still being authorized in parts of the state that have never had legal syringe access, such as Bakersfield and San Diego County. State funding for harm reduction staffing finally came through, with the California Harm Reduction Initiative (CHRI), thanks to the hard work of a lot of advocates around the state for the last couple of years. Finally, the State Office of AIDS issued a policy statement clarifying that smoking supplies such as pipes, were legal to distribute and possess, as a part of harm reduction efforts.