We say “needle exchange,” but open access—not one-for-one exchange—is best for health
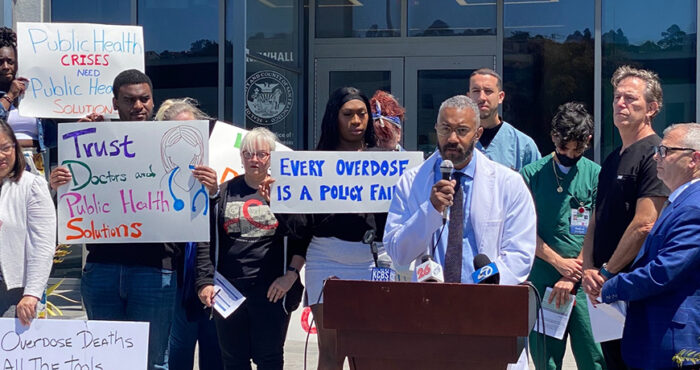
Overdose deaths from fentanyl-laced street drugs, outbreaks of hepatitis C and HIV among people who inject drugs, and other effects of the national opioid crisis have renewed the community’s focus on how best to help people who use drugs back. Fortunately, research and public health best practices developed in the early days of the HIV epidemic have informed the effective and rational response to the harms caused to those of us who use drugs—and our communities.
Needle exchange and syringe access programs combat the spread of infectious diseases among people who use injection drugs, improve participant health, and increase linkage to social services including drug treatment. In January 2016, Congress lifted the ban on federal funding for needle exchange and syringe access programs in response to the opioid epidemic, and some states have quickly grown needle exchange programs in response. There’s not always agreement on the best ways to serve people who inject drugs with supplies, or agreement on why people should support these services in their own community. Here’s some of what we know about syringe access from the research.
Syringe access and exchange benefits public health
The public health benefits to syringe access are clear. Syringe access programs across the U.S. have curbed the spread of infectious diseases like HIV and hepatitis C and also reduce the likelihood that people who inject drugs develop other bacterial infections and poor vein health.
In San Francisco, the percentage of people who used injection drugs and were infected with HIV doubled between 1986 and 1987—rising from 7% to 14%. When efforts were rolled out in the city to distribute syringes, test for HIV and educate people about how to sterilize injection equipment with bleach, the seroprevalence rate stabilized at about 12% from 1987 into the early 1990s.
The city of San Francisco, which continues to support a comprehensive syringe access program, sees some of the lowest rates of HIV transmission among people who inject drugs. Out of the estimated 22,500 people who inject drugs in San Francisco, a total of 21 contracted HIV in 2016 (that were not part of another risk group as reported by the Department of Public Health). The proportion of new HIV diagnoses occurring among people who inject drugs has hovered between 4% and 9% for the past 10 years.
User-driven syringe access benefits health the most
The models that govern syringe access and distribution—that dictate how many syringes a client can receive—make a big impact on how effective these harm reduction programs are. In other words, not all syringe exchange and access programs are equal.
Allowing clients to choose the number of needles they receive—syringe “access” as opposed to one-for-one “exchange”—has been found to be the most effective to prevent infections and the best way for people who inject to protect their own health.
“Distribution approaches to syringe exchanges have a larger impact on reducing syringe sharing and unsafe injection practices than one-for-one exchanges, and do not result in increased unsafe discard of syringes,” said Robert Heimer, PhD, a professor of epidemiology and pharmacology and director of emerging infections program at Yale School of Public Health. “This is the policy that works best.”
The distribution model is, as Heimer described, a ‘how many do you need?’ way of distributing syringes. “If someone says they need a case [of syringes], you give them a case,” he explained. One-for-one syringe exchanges are much stricter: People can get new syringes, but only to replace the exact number that are returned. Often, one-for-one exchanges also have a cap on the number of syringes that can be accessed at one time.
“If you don’t want people sharing equipment, you have to give people adequate supplies so that they never have to share,” said Terry Morris, director of the San Francisco AIDS Foundation 6th Street Harm Reduction Center. “When people save their syringes for reuse, because of scarcity, they’re more likely to loan them to someone else. If they immediately throw used syringes into a bio-bin for disposal, because they’re not worried about scarcity, they’re going to be safer.”
One-for-one exchanges and other policies that limit the number of syringes that people can access at one time make it more likely that people will end up re-using, or sharing, injection drug equipment, Heimer says. Hepatitis C is especially likely to be transmitted during the drug dissolving, cooking or injecting process—the virus is more resilient than HIV—so it’s crucial for sterile syringes to be used whenever people inject and prepare drugs, he said.
Syringe access reduces re-use
A study of syringe exchanges in San Francisco, Chicago and Baltimore conducted in the early 1990s measured syringe re-use over time to assess the impact of these fairly new exchange programs. In all three cities, the percentage of people who reported using a syringe only once before returning it increased over time. But in Chicago—the city that did not operate on a strictly one-for-one exchange—the percentage of people reporting only one injection per syringe went up dramatically (from 6.4% to 74.2%) while the two other cities saw less of an impact. (San Francisco saw a rise from 10% to 29% in the three years prior to 1993; Baltimore found that 3.2% of people used syringes once before accessing the exchange and 11.6% did 6 months later).
In the early nineties, Chicago allowed ten syringes to be distributed for the first five returned with no limit on the total number that could be exchanged but the other two cities at that time operated on a strict one-to-one exchange. The authors speculate that, “the [Chicago] approach may increase accessibility to the point where syringes can be routinely used just once.”
Another study, conducted between 1998 and 2000, compared drug-use practices among people in Chicago, Oakland and Hartford. The study found that people in cities with more permissive syringe access policies that allow for greater access (Chicago and Oakland) were significantly less likely to reuse syringes than people who were only able to get syringes one-to-one with a limit capped at 10 (Hartford). People who used syringe exchange sites were also less likely to have injected drugs using someone else’s previously used syringe in Chicago (7%) and Oakland (11%) compared to Hartford (26%).
“No one likes using the dirties”
A recently published report of peer-based qualitative research done with people who inject drugs in Australia makes is clear that people prefer not to re-use syringes. “No one likes using the dirties,” the report sums. But participants were very clear that re-use did happen when restrictions were placed on the number of syringes people could access per day. “‘They tell you are only allowed six [syringes] a day, but some days I have more, might have eight or nine shots a day…they’re telling me how many shots I can have a day and that doesn’t work out,’” the report quotes one participant as saying.
One-for-one exchange doesn’t mean fewer improperly discarded syringes
One-for-one exchanges, and other policies that limit the number of syringes that people can access, were developed with the idea that fewer syringes would be improperly discarded when the number of syringes people can access is limited to the number of used syringes they return.
“This has never been shown to be true,” stated Heimer. He points to city-level data conducted in three cities across the U.S.—each with different syringe exchange/distribution policies—that compared rates of syringe return. The city with the most liberal policy—Chicago—also had the highest rate of return of syringes. “Even though they were giving away more syringes, a higher percentage of the syringes came back. Giving out more does not mean those syringes disappear into the ether. If you give more syringes away, you reduce syringe scarcity and more of them come back,” he said.
Another study conducted across 24 syringe exchange sites in California also found that greater syringe access did not increase unsafe syringe disposal. In fact, the greater the access to syringes, the more likely people are to dispose of them in safe locations.
Comparing two cities with different syringe access policies, a study by Hansel Tookes and colleagues in 2012 found that San Francisco—a city with syringe access programs—had a much lower density of improperly discarded syringes than Miami, a city that at the time had no syringe access programs. In a survey with participants in both cities, 1% of people who used injection drugs in San Francisco reported discarding syringes in a public place in the previous 30 days, while 45% reported doing so in Miami. In San Francisco, 80% of all syringes were disposed at syringe access locations.
“We found eight times the number of syringes on walkthroughs in Miami as compared to San Francisco. Our surveys of IDUs [injection drug users] in both cities corroborated the walkthrough data, showing that IDUs in Miami are much more likely to dispose of syringes in public places than IDUs in San Francisco… These results suggest that NSPs [needle and syringe programs] are a significant means of collecting used syringes and do not increase the amount of publically discarded used syringes,” the authors said.
Sources
Blumenthal, R. and others. Sterile syringe access conditions and variations in HIV risk among drug injectors in three cities. Addiction, 2004.
Blumenthal, R. and others. Higher syringe coverage is associated with lower odds of HIV risk and does not increase unsafe syringe disposal among syringe exchange program clients. Drug and Alcohol Dependency. 2007.
Duvnjak, A. and others. ‘No one likes using the dirties.’ Australian Injecting and Illicit Drug Users League. 2015.
Heimer, R. and others. Syringe use and reuse: Effects of syringe exchange programs in four cities. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1998.
Lurie, P. and others. The public health impact of needle exchange programs in the United States and abroad: Summary, conclusions and recommendations. 1993.
Tookes, H. E. and others. A comparison of syringe disposal practices among injection drug users in a city with versus a city without needle and syringe programs. 2012.
Watters, J. Trends in risk behavior and HIV seroprevalence in heterosexual injection drug users in San Francisco, 1986-1992. JAIDS, 1994.