How do meth and other stimulants affect viral suppression?
For many years, researchers have observed that people using stimulants (such as meth, powder cocaine, and crack-cocaine) who are living with HIV are less likely to stay engaged in HIV care, are more likely to have higher viral loads and are more likely to experience faster disease progression. But in the age of universal HIV treatment with powerful and effective antiretrovirals, the impact of stimulant use on HIV treatment appears to be less significant than it once was.
Adam Carrico, PhD, from the University of Miami, joins BETA to discuss new research his team published about the impact of stimulant use on viral suppression, and share some take-aways from his research to improve the health of people living with HIV who use stimulants like meth.
BETA: Thanks for sharing information about your research, Adam. Could you start by talking a little bit about why it’s important to understand the effects that stimulants have on HIV health and viral suppression?
Adam Carrico, PhD: This work is important for a couple of reasons. For one, viral suppression is just as important for people who use stimulants as it is for anyone else. Having a better understanding of the challenges that people who use stimulants may face in becoming undetectable will may ultimately help us increase rates of viral suppression in this high-priority population.
People who use substances, particularly people who use meth, are also more likely to engage in sexual risk behaviors including HIV transmission risk behavior. If people are able to stay undetectable, this is one of the best tools that we have for preventing the onward transmission of HIV. All of this work is nested in the double benefit of HIV treatment as prevention by optimizing the heath of people who use stimulants and reducing risk of onward HIV transmission.
What effect did stimulants have on viral suppression for people living with HIV in your research?
In collaboration with a team of investigators at the University of California, San Francisco (UCSF), the study published recently in JAIDS compared the rates of viral suppression between people who used stimulants (meth, powder cocaine, crack-cocaine or cocaine injection) and people who didn’t use stimulants.
We included 1,635 people living with HIV who were part of the SCOPE clinical cohort at Zuckerberg San Francisco General Hospital, which began enrolling people in the year 2000. Basically, we looked at rates of viral suppression and compared people who reported no stimulant use, those who reported stimulant use at half of the study visits, and those who reported stimulant use at every visit. We also looked at the differences in rates of viral suppression between these groups in the years before universal HIV treatment (2000 – 2009) and following the advent of universal HIV treatment (2010 – 2016).
Across all of the years, people who used stimulants were less likely to be virally suppressed than people who did not report stimulant use. But these differences were diminishing in the era of universal HIV treatment. Basically, our research found that stimulants seem to be affecting rates of viral suppression less in the current day and age than in previous years. By no means is the problem solved, but things appear to be better than they used to be.
Why do you think stimulant use seems to be having less of an effect on viral suppression these days compared to previous years?
This isn’t something that we collected data on in this study, but we do know that over the years HIV medications have gotten better. You can take one pill once a day now. The medications are also more forgiving of non-adherence—people can get virally suppressed even at moderate levels of adherence. That is likely one reason why we see that people using stimulants are more likely to be virally suppressed in recent years.
Another reason may be that people are more motivated to become undetectable now that we know that undetectable equals untransmittable (U=U). People are motivated to be undetectable knowing that they can meet romantic and sexual partners without having to worry about onward HIV transmission.
What message do you have for people living with HIV who use stimulants?
After working with guys in San Francisco who use meth and also women in Miami who use cocaine, I would say that just because you’re using stimulants doesn’t mean you can’t take your HIV medications. Even if you’re partying, make sure to take your medications so you can be undetectable.
The other major take-home is that viral suppression isn’t the only thing to consider health-wise. It’s great if you’re undetectable. Research by my team and others shows that stimulants may be detrimental to the immune system even if people are undetectable. Stimulants can still damage the immune system in important ways that can increase risk for negative health outcomes. Viral suppression is just one metric. So, reducing or abstaining from stimulant use can improve your health even if you are already undetectable.
Can you tell us more about the focus of your research now and in the future? What more is there to find out about stimulant use and HIV health?
My team is developing and testing interventions that amplify or accelerate the benefits of HIV treatment as prevention in people who use stimulants like meth. We’re testing approaches that help people get a handle on their stimulant use in the hopes that it will also have benefits for people’s ability to manage HIV medications and be undetectable.
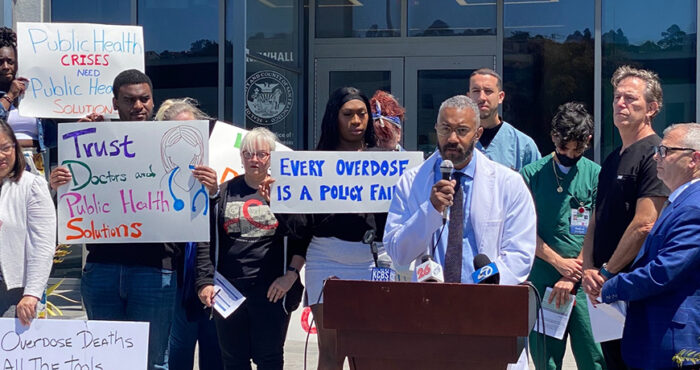
One intervention we developed is a brief therapeutic intervention that helps people in substance use treatment focus on positive affect like happiness or gratitude to find ways that life is rewarding and pleasurable outside of their substance use. This research was conducted in partnership with the Positive Reinforcement Opportunity Project (PROP), which is administered by the Stonewall Project at San Francisco AIDS Foundation.
Inspired by harm reduction, the orientation of the positive affect intervention is very different than mainstream substance use treatment approaches—which tend to focus on avoiding triggers or demanding abstinence. Instead of focusing on taking things away, we’re helping people add something positive to their lives, so that hopefully the substance use becomes less of a dominant focus. It’s about how to find pleasure outside of substance use, and making your life more rewarding and meaningful. Our recent findings show that this approach reduces methamphetamine craving and self-reported stimulant use in HIV-positive, meth-using men and trans women receiving services at PROP.
Source
Carrico, A. W. and colleagues. Stimulant use and viral suppression in the era of universal antiretroviral therapy. JAIDS, January 2019.
Want to talk to someone about drugs or alcohol?
The Stonewall Project is here to help. Stonewall offers free harm reduction counseling to gay, bi and trans men who want to assess their substance use and are thinking about making changes. For more information and to seek services, visit stonewallsf.org or call 415-487-3100.