Since breast milk can contain HIV, U.S. perinatal guidelines state that women with HIV should not breastfeed, and instead feed their babies with formula or banked breast milk. Without antiretroviral therapy (ART), the risk of HIV transmission from mother to baby during breastfeeding is about 16%. Even if the mother, baby, or both are on antiretrovirals (ARVs), there’s still some risk of transmission, with estimates ranging from 1.1% to 5.4%. But what if mothers aren’t willing to give up the idea of breastfeeding their baby?
Some clinicians say that simply informing women with HIV not to breastfeed actually facilitates covert breastfeeding that’s not done under the care or guidance of a clinician.
“Our concern was that we were driving it underground by, in the U.S., by saying, ‘don’t breastfeed.’ And some of our women would intermittently breastfeed. When we would ask them if they were formula feeding, they would say ‘yes,’ and not acknowledge that they were perhaps doing mixed feeding,” said Judy Levison, MD, MPH, associate professor of obstetrics and gynecology at Baylor College of Medicine.
The problem with intermittently breastfeeding—what clinicians call ‘mixed’ feeding, or going back and forth between formula and breastfeeding—is that it appears to have a higher associated risk of HIV transmission than only breastfeeding. Many studies have investigated the issue, with one study of 958 babies born to women with HIV in Zambia finding a more than three-fold increased risk of early postnatal HIV transmission with mixed feeding compared to exclusive breastfeeding.
While it’s not entirely clear why this is the case, Levison says that there are a few theories. There’s evidence that formula irritates the baby’s gut and may open up “microportals” that provide an easier entry for HIV when breast milk containing HIV is ingested following formula. A more recent theory is that women who only breastfeed intermittently are more likely to have engorged breasts and breast inflammation, which increases the amount of virus that they shed in their breast milk.
“[The increased risk] probably comes from some combination of maternal factors and infant factors, and it’s a much more complicated issue particularly for women on ARVs,” said Deborah Cohan, MD, MPH, the medical director for the Bay Area Perinatal AIDS Center. “There’s a study that suggests that it’s not mixed feeding itself that’s the risk factor, but what really matters is how much virus the baby is exposed to the in the setting of breastfeeding. It depends on how much milk the baby actually ingests, how much virus is in the milk, with the added piece of how much at risk the baby is in terms of if there’s gut inflammation.”
What can clinicians do for women who want to breastfeed?
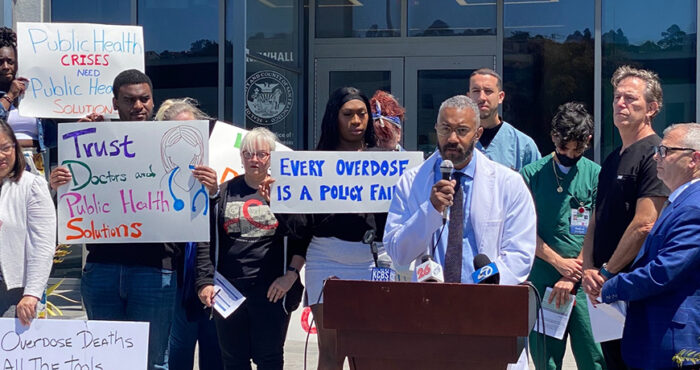
Clinicians and community health specialists discussed this issue during a webinar held by the San Francisco Department of Public Health. Consider the case, said Levison, of a pregnant woman who has been newly diagnosed with HIV who says the hardest part of adjusting to her new diagnosis is not being able to breastfeed. “She believes breastfeeding provides the best nutrition, immune support and optimal bonding. We say, ‘In the U.S., it is not recommended for a woman with HIV to breastfeed. Is that an issue or problem for you?’ We have been surprised by how often tears start rolling down faces, and a frank discussion follows.”
If a mother still wishes to breastfeed even after learning about the risk of HIV transmission to her baby, Levinson applies a harm reduction approach. She does this, she says, with the understanding that people will make positive health choices if they are provided adequate support, empowerment and education.
There are options to reduce the risk that a woman will pass on HIV while breastfeeding, Levinson says. She ensures that the mother is virally suppressed and knows about the option for her baby to be provided ARV prophylaxis beyond the standard 6-week course typically given to babies born to women with HIV. She explains that “fairly rapid” weaning lowers risk of transmission as does exclusive—as opposed to mixed—breast feeding. She asks women to look for—and immediately come in for care—if there are signs of mastitis, since inflammation of the breast tissue comes with a greater risk of HIV shedding. And she does viral load tests on mothers monthly and HIV tests on the baby every month as well and then 1, 3, and 6 months after weaning.
There’s still more to learn about risk associated with breastfeeding—especially for mothers on highly-active ARVs who have suppressed viral loads. For instance it’s not yet clear, said Cohan, how different viral loads are between a woman’s blood and her breast milk.
But, Cohan concluded, “I believe that women can hold subtlety and can hold contradiction. And that, in clinical care, I believe it is our obligation to include women in the discussion about what’s safe and not safe and best for them as the data accumulate. And work with women to integrate these data in their own lives.”
For more information
Visit the HIVE website for more resources specific to HIV-positive women including real-life stories and an summary of infant feeding basics.
Call the National Perinatal HIV Hotline at 1-888-448-8765 for a free clinical consultation on all aspects of perinatal HIV including infant care.
Listen to the webinar, A woman-centered approach to infant feeding and HIV.
Sources
Coovadia, H. M. and others. Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding in the first 6 months of life: an intervention cohort study. The Lancet, March 2007.
Kuhn, L. and others. High Uptake of Exclusive Breastfeeding and Reduced Early Post-Natal HIV Transmission. PLoS One, 2007.
Neveu, D. and others. Cumulative exposure to cell-free HIV in breast milk, rather than feeding pattern per se, identifies postnatally infected infants. Clinical Infectious Diseases, 2011.
Nduati, R. and others. Effect of breastfeeding and formula feeding on transmission of HIV-1: a randomized clinical trial. JAMA, March, 2000.
Shapiro, R. L. and others. Antiretroviral Regimens in Pregnancy and Breast-Feeding in Botswana. The New England Journal of Medicine, June, 2010.
The Kesho Bora Study Group. Triple antiretroviral compared with zidovudine and single-dose nevirapine prophylaxis during pregnancy and breastfeeding for prevention of mother-to-child transmission of HIV-1 (Kesho Bora study): a randomised controlled trial. The Lancet, March 2011.