Broadly neutralizing antibody PGT121 reduces hidden viral reservoir
A broadly neutralizing antibody known as PGT121, when used with an immune stimulant, may be able to target and help eliminate the hidden HIV reservoir, according to a study in monkeys presented at CROI 2018. These findings could contribute to the development of an effective HIV cure or a strategy to keep HIV in remission.
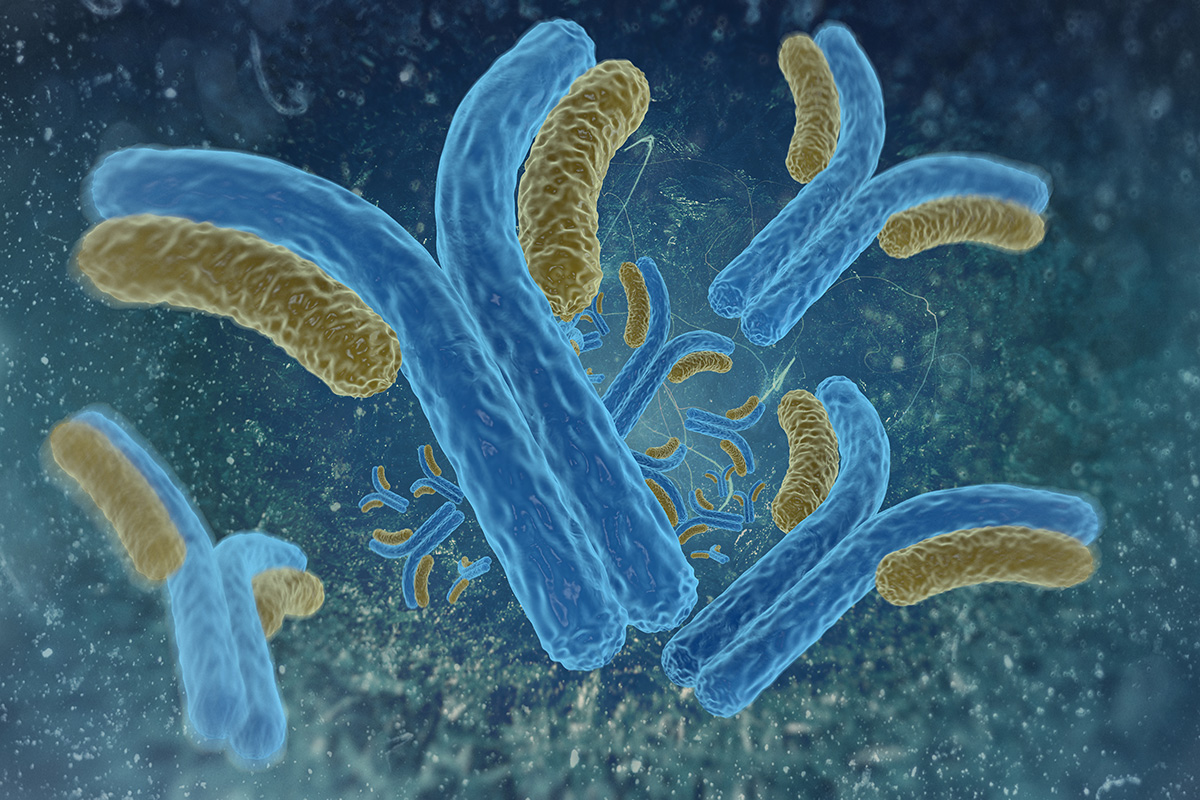
Most antibodies (which are part of the body’s defense system) can only target one strain of one type of virus. But broadly neutralizing antibodies (bNAbs), such as PGT121, are able to bind to a high percentage of virus strains. For that reason, they are hopeful as an HIV cure strategy since they may be able to keep pace with HIV, which mutates rapidly.
Previously, studies with human participants have showed that bNAbs can delay viral rebound if given when HIV antiretroviral therapy (ART) is discontinued.
Can bNAbs target the viral reservoir?
The viral reservoir–in locations throughout the body–refers to dormant virus that lingers even when antiretroviral medications are taken. The viral reservoir is the reason why people who stop taking HIV medications see a return in viral loads once medication is stopped–in other words, it’s what stands in the way of an HIV cure.
In this study, Dan Barouch, MD, PhD and colleagues investigated the ability of bNAbs to target and mark for destruction HIV that is part of the viral reservoir.
To test this, the researchers administered bNAbs during ART suppression, but then stopped and waited until the bNAb levels were no longer at therapeutic levels at the time of ART discontinuation. The bNAbs were active only during the time that ART was suppressing viral loads too—so any effect on viral rebound caused by the bNAb therapy could be attributed to the therapy’s effects on the viral reservoir.
The researchers found that infusions of PGT121 plus an immune stimulant known as GS-9620 into simian human immunodeficiency virus (SHIV) infected monkeys delayed viral rebound for approximately one to two months after ART was stopped.
Because the bNAb therapy was not active after ART was stopped, the only way for this effect to have happened would be if the bNAb therapy destroyed virus in the reservoir.
“Our findings suggest that the development of interventions to activate and eliminate a fraction of the viral reservoir might be possible,” said Barouch in a study press release. “Although we are still a long way off from having a cure for HIV, our data suggest a strategy for targeting the viral reservoir that can be further explored.”
Details of the study
The study included 44 rhesus macaques who were infected with simian human immunodeficiency virus (SHIV), a virus that is similar to HIV and which is often used in non-human primate studies.
After SHIV infection, all monkeys showed similarly high viral loads at week 1. The monkeys were then started on daily antiretroviral therapy at day 7, achieved undetectable viral loads, and were kept on antiretroviral therapy for 96 weeks.
The 44 monkeys remained on treatment and were divided into four groups that received:
- Five infusions of the HIV bNAb known as PGT121, once every two weeks beginning at week 106 until week 114
- Ten administrations of GS-9620, an immune stimulant by Gilead Sciences, once a week beginning at week 96 until week 114
- Both therapies, PGT121 plus GS-9620, on the dosing schedules outlined above
- Neither therapy (the control group)
After week 114, the researchers allowed for a washout period, during which time neither the PGT121 nor GS-9620 were administered. The monkeys continued receiving antiretroviral therapy until week 130 when treatment was stopped.
PGT121 levels in the blood, lymph nodes, and colorectal biopsies were undetectable between week 120 and 122 for both groups receiving PGT121. This confirmed that there was no PGT121 antiviral activity at the time of ART discontinuation, which is important for determining whether the bNAb reduced the viral reservoir.
Results of the study
At week 130, all ART was stopped and the researchers looked for viral rebound over 160 days after stopping ART.
In the control group, virus rebounded in 100% of the control animals between day 14 and 42. The control monkeys had high peak point viral loads (highest viral load after rebound) and moderate set point viral loads (viral load after it has settled or stabilized).
In the GS-9620-alone group, 10 out of 11 monkeys experienced rebound at a median of 21 days. These monkeys had similar viral loads to the control group.
In the PGT121-alone group, nine out of 11 monkeys rebounded at a median of about 80 days. A number of these monkeys rebounded late and had lower viral loads.
In the combination group, only six out of 11 monkeys rebounded and most of them had substantially delayed viral rebound, at a median of 121 days. They also showed reduced peak and set point viral loads. At the end of the 160 days, nearly half (five out of 11) of the combination group did not show any viral rebound.
The researchers then conducted what’s called an adoptive transfer study, where they take cells from an infected animal and transfer them into an uninfected animal to test whether there’s any virus that can replicate. They wanted to see if the animals that did not rebound still had recoverable virus.
The researchers harvested cells from the lymph nodes and blood from the animals that did rebound and transferred the cells into uninfected monkeys. Remarkably, this did not transfer infection, suggesting that the amount of residual replication-competent virus in the GS-9620/PGT121-treated animals was extraordinarily low.
The researchers also looked at viral DNA at week 120 (before ART discontinuation at week 130). Viral DNA was below the sensitivity of the assay (undetectable) in all groups when the blood was measured. Barouch believed that this was probably because the monkeys were started on ART very soon after infection. However, when measuring the lymph nodes, the researchers were still able to detect viral DNA in the majority of the controls, but there were substantially less viral DNA levels in the combination group, suggesting that their viral reservoirs had been reduced.
Will this be studied in humans?
“HIV excels at evading the immune system by hiding out in certain immune cells. The virus can be suppressed to very low levels with antiretroviral therapy, but quickly rebounds to high levels if a person stops taking medications as prescribed,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID), in a statement. “The findings from this early stage research offer further evidence that achieving sustained viral remission without daily medication might be possible.”
Barouch noted that other studies find that, compared to other bNAbs, PGT121 is particularly robust at binding activated HIV-infected CD4 T cells and inducing antibody functions, which may help clear infected cells.
The mechanisms behind the delayed rebounds (and absence of rebounds) in the combination group remain unclear, but the results suggest that bNAbs combined with an immune stimulant may be able to target the viral reservoir.
Barouch said that the results perhaps would not be as profound had they not started with animals that were treated very early during acute HIV infection. But he noted that a study using PGT121 and GS-9620 in chronically infected monkeys is ongoing.
While the results are promising, humans don’t always show the same results as seen in animal studies. Further research is needed to determine safety before testing the GS-9620 and PGT121 combination in humans.
Source
Barducci, E. and colleagues. PGT121 combined with GS-9620 delays viral rebound in SHIV-infected rhesus monkeys. CROI, 2018, Abstract 73LB.